Digital technology is used throughout UAB Medicine for virtual visits, remote patient monitoring, treatment procedures, collecting and using patient data, and much more. In recent years, nursing at UAB Medicine has made greater use of telehealth with approaches that are here to stay – at the bedside, in clinics, and in patients’ homes. These new approaches also help nurses provide more flexible patient care and make better use of the knowledge that experienced nurses have.
Prepping patients
Some UAB Medicine clinics have dedicated telehealth platforms, while others run on a hybrid model that combines virtual and in-person visits. Nurses assist clinic operations through “pre-loading” patients for virtual and follow-up visits by collecting patient information and recording intake notes. Nurses or telehealth educators walk patients through using telehealth platforms and connect them with other resources as needed.
“Clinic nursing staff are able to assess patients and assist with navigating care through an appropriate visit type that meets the needs of the patients,” says UAB Medicine Director of Clinical Services Rosemary Ryan. “We are expanding the capacity of some clinics that had otherwise been limited by physical space. Meanwhile, the patients who need in-person care are getting it more efficiently.”
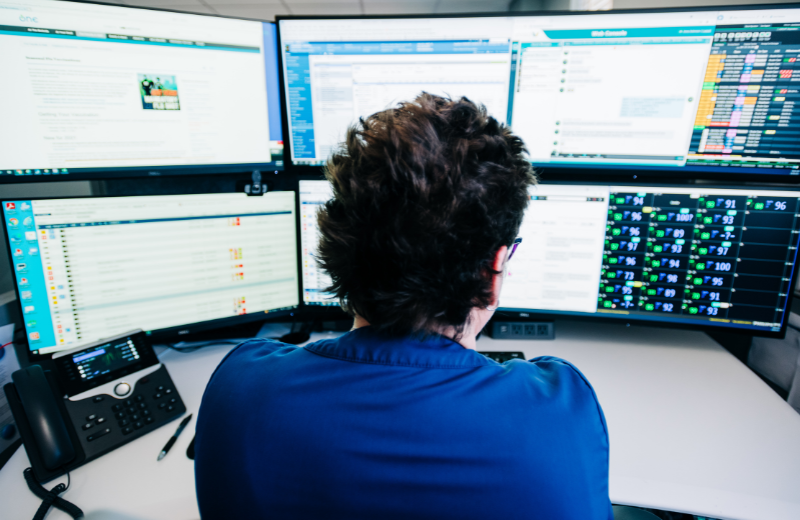
Patient Healthcare Coordination Center
UAB Medicine’s Patient Healthcare Coordination Center (PHCC) is another virtual nursing success for ambulatory care. The PHCC triages calls and messages from patients, caregivers, and care team members. Its nurses also are responsible for some remote patient monitoring and telehealth visits, as well as coordinating with pharmacy services.
“The PHCC consolidates nursing knowledge and provides health care resources and medical support for the coordination of patient care,” Ryan says. “It’s also a different way for nurses to work and remain in direct patient care but in a remote capacity.”
Remote patient monitoring
UAB Medicine’s Remote Patient Monitoring (RPM) program is part of the PHCC and has a dedicated team of nurses who receive and monitor transmitted health data from patients enrolled in RPM. The RPM team supports over 400 patients using Bluetooth technology and mobile monitoring devices, and these nurses work with providers to manage certain chronic medical conditions while patients are in their homes.
Alabama has high rates of diabetes and heart disease, and data related to these conditions can easily be collected remotely and flagged for concerns. “We can be proactive by preventing readmissions and decreasing unnecessary Emergency Department visits,” Ryan says. “This is a win for UAB’s population health efforts.”
Patient access and experience
Expanding telehealth services makes it easier for patients to receive care, and it opens the door for those in rural areas who might have limited access to medical care – especially from specialists.
“When a patient is unable to attend a scheduled appointment, it impacts both the patient and the organization, and virtual options help prevent barriers or lessen the impact on patient flow and access to care,” Ryan says. “For example, immunocompromised patients and those at high risk for falls can often receive care from home. Appropriate telehealth services can improve the patient experience and provide more timely and efficient access to care, but this does not replace in-person visits when they are needed.”
More knowledge at the bedside
Tele-ICU Nurse Manager Paul Malito says telehealth helps accomplish two key goals for inpatient care: proactively addressing changing patient conditions, and making more efficient use of experienced nurses’ knowledge. Three new inpatient platforms take advantage of in-room technology that allows constant virtual monitoring and interaction to better respond to symptoms. These platforms include Tele-ICU, Tele-Acute Nursing, and the Virtual Sitter Program. Over 320 UAB Hospital patient rooms are wired with virtual patient monitoring equipment that enables nurses to observe and interact with patients with audio and/or video, communicate with bedside nurses, and engage emergency alarms. Also, 24 mobile carts are available to bring this technology to other rooms as needed.
New roles for experienced nurses
Malito says the lack of bedside experience among nurses is a problem nationally. On average, nurses have fewer than six months of bedside experience, and that has been further limited by the COVID-19 pandemic over the past three years. An operations center for the Tele-ICU and Tele-Acute Nursing units connects less experienced bedside nurses with those who have more experience.
“On average, the nurses working in this virtual operations center have more than 16 years of experience,” Malito says. “Many of these nurses, who have decades of experience and mental vigor, were close to retirement, because the physical rigors of bedside care were taking a toll on their bodies. Having the option to work in a virtual operations center may extend their career another 4-5 years, because they can continue to utilize their nursing minds without the stress on their bodies.”
These nurses help oversee common care tasks, such as interpreting lab reports, choosing IV medications, clarifying clinical notes, and deciding when to call for support.
Malito recalls an early example of the effectiveness of Tele-ICU nurses. Recently, a new nurse in one of the Tele-ICU monitored units was caring for a patient who was on a ventilator and in distress. The nurse was trying to make the patient more comfortable and needed an experienced nursing opinion to help carry out a titration order for a medication. The Tele-ICU nurse was able to join at the bedside by video monitor, provide guidance, and remain engaged, so that the new nurse would not be alone. A crisis may have been averted, and a new bedside nurse was able to learn with limited stress, he says.
Staying focused on patients
“Bedside nurses can be under tremendous stress managing the care of multiple patients,” Malito says. “We can take some of the mental load off of them as new patients arrive by helping read doctors’ notes, interpreting charts, and clarifying providers’ care plans even when they don’t have orders set up or have changed orders.”
This arrangement also can improve patient satisfaction by reducing the amount of time before new patients are engaged by staff. Nurses from the Tele-ICU sometimes connect with newly admitted ICU patients immediately to complete the admission process, provide information, and offer the assurance of constant monitoring. In fact, Malito says the positive results of Tele-ICU are reflected in quarterly reports through lower mortality rates, greater patient satisfaction, and shorter hospital stays.
Virtual sitters
UAB Medicine introduced the Virtual Sitter program in September 2022 to provide an additional layer of support to help keep patients safe. The program empowers specially trained support staff to monitor patients remotely via video camera and reduces the number of sitters deployed to the bedside.
Virtual sitters are trained to notice potential patient safety risks and communicate quickly and confidently to the patients via speaker while deploying resources to the bedside to keep the patient safe. Virtual sitters can reduce falls by 30% and are becoming the standard of care at high-performing hospitals. From a nursing point of view, this innovation allows members of the nursing team to provide care to multiple patients while helping ensure that high-risk patients still have a watchful eye.
In short, telehealth technology gives nurses and patients greater flexibility. Still, these new capabilities rely on knowledgeable nurses who are committed to excellent patient care.
“Telehealth means a future with better and more accessible patient care, flexible career options for nurses, and more working across teams to use data in new ways,” Malito says. “It isn’t changing us as nurses, but it is enhancing what we already do well.”
This story is part of the Nursing Annual Report 2022. Click here to view the report.
